Pharmaceutical manufacturing
1. Automation in Pharmaceutical Manufacturing 1.1. Introduction to Automation in Pharmaceuticals 1.1.1 What is Automation? Automation involves using machines, control systems, and software to perform tasks with minimal human intervention. In pharmaceutical manufacturing, it encompasses everything from production lines to quality control. 1.1.2 Why is Automation Important? Pharmaceutical manufacturing demands high accuracy and compliance with […]
“Revolutionizing Pharmaceutical Manufacturing: The Crucial Role of Blockchain in Ensuring Traceability”
1. Introduction Pharmaceutical manufacturing is a cornerstone of the healthcare industry, ensuring the production of high-quality medicines that improve and save lives. However, challenges such as counterfeit drugs, supply chain inefficiencies, and regulatory compliance pose significant risks. Blockchain technology has emerged as a transformative solution, enhancing traceability, transparency, and trust within the pharmaceutical supply chain.
“Navigating Challenges: Effective Strategies for Managing Risk in Pharmaceutical Manufacturing”
1. Understanding Risks in Pharmaceutical Manufacturing 1.1. The Importance of Risk Understanding 1.1.1 Why Risk Awareness is Critical 1.1.2 Role of Risk Understanding in Decision-Making 1.2. Types of Risks in Pharmaceutical Manufacturing 1.2.1 Product Quality Risks 1.2.2 Operational Risks 1.2.3 Regulatory Risks 1.2.4 Supply Chain Risks 1.2.5 Environmental and Safety Risks 1.2.6 Cybersecurity Risks 1.3.
“Ensuring Excellence: The Crucial Role of Data Integrity in Pharmaceutical Manufacturing”
1. Understanding Data Integrity Data integrity refers to the accuracy, completeness, and consistency of data throughout its lifecycle. It ensures that data, whether in electronic or paper-based formats, is reliable and trustworthy. In the pharmaceutical industry, this includes manufacturing records, laboratory test results, and quality assurance documentation. 1.1 ALCOA+ Principle The ALCOA+ principle underpins data
“Navigating the Challenges of 3D Printing in Pharmaceutical Manufacturing”
1. Introduction 3D printing, also known as additive manufacturing, has emerged as a revolutionary technology in many industries, and the pharmaceutical sector is no exception. This technology, which creates objects layer by layer from digital models, holds the potential to reshape pharmaceutical manufacturing by enabling the development of personalized medicines, improving drug delivery systems, and
“Navigating the Challenges of 3D Printing in Pharmaceutical Manufacturing” Read More »
“Pharmaceutical Manufacturing Outsourcing: Benefits and Challenges Explored”
1. What is Pharmaceutical Manufacturing Outsourcing? Pharmaceutical manufacturing outsourcing involves contracting third-party organizations, known as contract manufacturing organizations (CMOs) or contract development and manufacturing organizations (CDMOs), to handle various stages of drug production. This can include: 2. Pros of Pharmaceutical Manufacturing Outsourcing 2.1. Cost Efficiency One of the primary drivers of outsourcing is cost reduction.
“Pharmaceutical Manufacturing Outsourcing: Benefits and Challenges Explored” Read More »
“Advancing Quality Control in Pharmaceutical Manufacturing: Techniques, Best Practices, and Future Trends”
1. Importance of Quality Control in Pharmaceuticals 1.1 Ensuring Patient Safety Quality control ensures that medications are free from contaminants, contain the correct ingredients, and meet the required potency levels to safeguard patient health. 1.2 Regulatory Compliance Pharmaceutical products must adhere to strict regulatory standards set by organizations such as the FDA, EMA, and WHO.
“Transforming Pharmaceutical Manufacturing: The Role and Impact of Sustainability”
Sustainability is reshaping pharmaceutical manufacturing, addressing environmental, social, and economic challenges while ensuring long-term industry viability. By adopting green chemistry, energy-efficient technologies, and waste reduction strategies, companies significantly reduce their carbon footprint and resource consumption. These practices not only mitigate environmental damage but also improve public health by curbing pollution. Moreover, sustainability fosters equitable access to medicines, promotes ethical labor standards, and strengthens community engagement. While the transition to sustainable practices poses challenges like high initial costs and regulatory complexities, the benefits—ranging from operational efficiency to enhanced societal trust—far outweigh the hurdles. Ultimately, sustainability drives innovation, accountability, and resilience, positioning the pharmaceutical sector as a vital contributor to a healthier planet and society.
“Transforming Pharmaceutical Manufacturing: The Role and Impact of Sustainability” Read More »
“Revolutionizing Pharmaceuticals: How AI is Transforming Manufacturing Processes”
1. The Role of AI in Pharmaceutical Manufacturing AI leverages advanced algorithms and machine learning techniques to analyze vast datasets, identify patterns, and provide actionable insights. In pharmaceutical manufacturing, this capability is being utilized across various stages of the production process, from research and development (R&D) to quality control and supply chain optimization. 2. Enhancing
“Revolutionizing Pharmaceuticals: How AI is Transforming Manufacturing Processes” Read More »
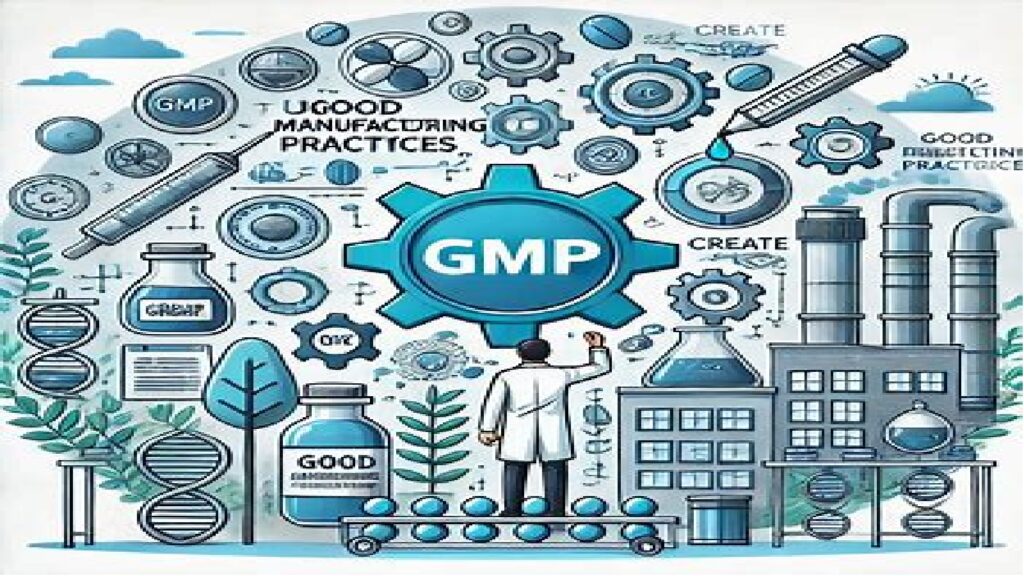
“Comprehensive Guide to Understanding Good Manufacturing Practices (GMP) in Pharma”
1. What Are Good Manufacturing Practices (GMP)? GMP refers to a set of regulations, codes, and guidelines that govern the manufacturing processes and environments in the pharmaceutical industry. These practices are enforced by regulatory bodies such as: GMP guidelines ensure that pharmaceutical products are consistently produced and controlled to meet predefined quality standards. 2. Importance
“Comprehensive Guide to Understanding Good Manufacturing Practices (GMP) in Pharma” Read More »